Understanding Venous Stasis Causes: Insights for Better Vascular Health
Venous stasis, a condition characterized by the slow flow of blood in the veins, can lead to a myriad of health complications. Understanding its causes is essential for prevention and treatment. This article aims to provide comprehensive insights into the various factors that contribute to venous stasis, how they affect vascular health, and effective strategies for management.
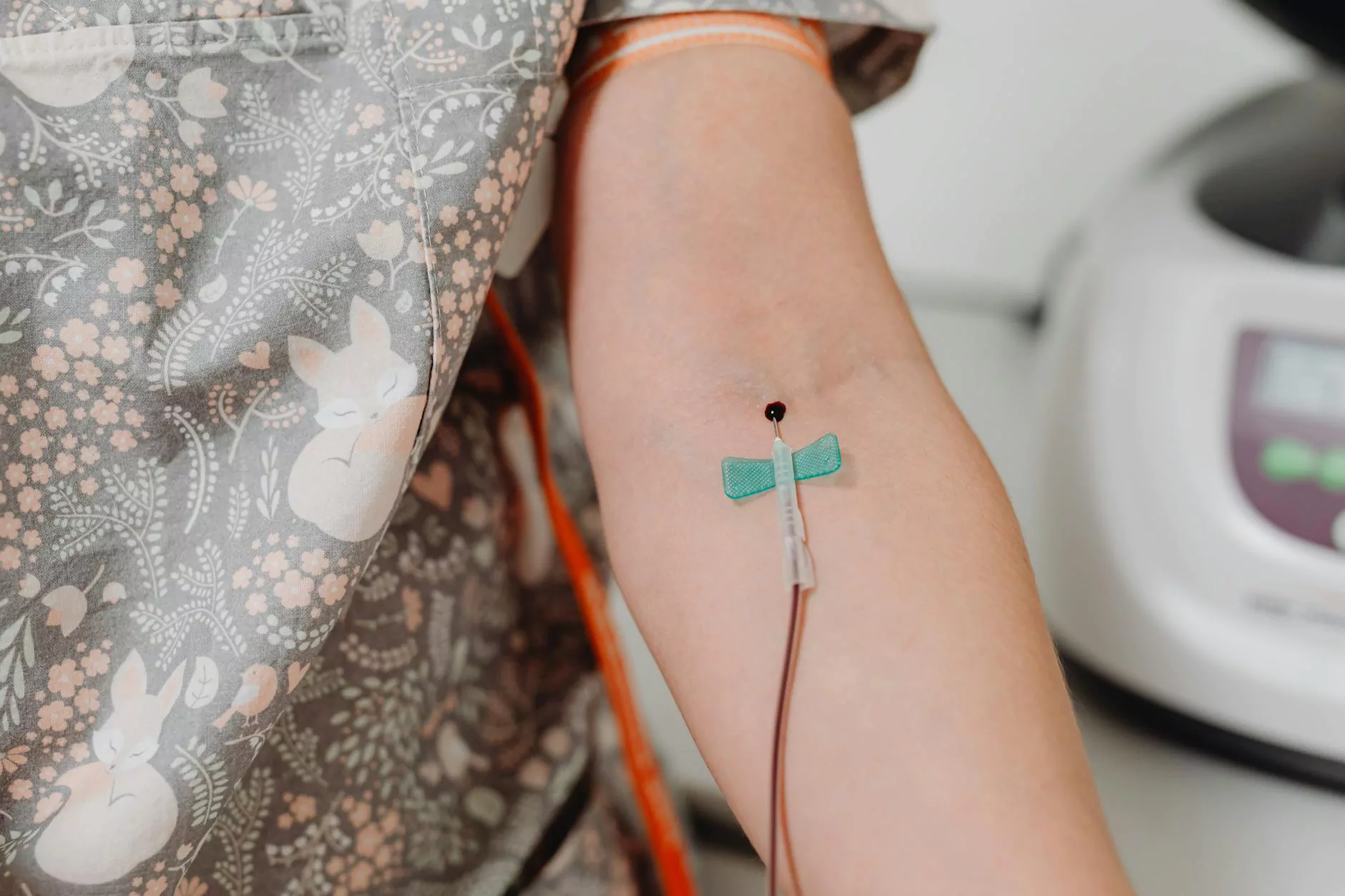
What is Venous Stasis?
Venous stasis occurs when blood pools in the veins, particularly in the lower extremities. This stagnation can lead to various complications, including swelling, pain, and even serious conditions like deep vein thrombosis (DVT). Recognizing the underlying causes is crucial for both patients and healthcare professionals.
Common Causes of Venous Stasis
Several factors can trigger venous stasis. Understanding these causes allows individuals to take proactive measures to maintain their vascular health.
1. Prolonged Inactivity
One of the most significant contributors to venous stasis is prolonged inactivity. Sedentary lifestyles—for example, long hours of sitting at a desk or prolonged periods of bed rest—can impede blood flow.
- Work Environment: Office jobs that require sitting for extended periods can hinder circulation.
- Travel: Long flights and car rides can also contribute to stasis due to lack of movement.
2. Obesity
Obesity significantly impacts vascular health and is a major risk factor for venous stasis. Excess body weight increases pressure on the veins, making it more challenging for blood to return to the heart. This pressure can lead to the weakening of vein walls and valves.
- Increased Vein Pressure: Body weight exerts additional pressure on the venous system.
- Hormonal Factors: Fat tissue can influence hormone levels, affecting vascular health.
3. Age
Aging naturally affects vein elasticity and valve function. As individuals age, veins can become less effective at returning blood to the heart, increasing the risk of venous stasis.
- Decreased Elasticity: Age-related changes can lead to less resilient veins.
- Degeneration of Valves: Older adults tend to have weakened vein valves.
4. Pregnancy
Pregnancy introduces various physiological changes, including increased blood volume and hormonal changes, which can lead to the development of venous stasis. As the uterus expands, it can put pressure on the pelvic veins, impediments blood flow.
- Increased Blood Volume: More blood circulating can overwhelm the venous system.
- Pressure from the Uterus: As the pregnancy progresses, the growing uterus compresses veins.
5. Medical Conditions
Certain medical conditions can predispose individuals to venous stasis. These include:
- Varicose Veins: Enlarged veins can lead to blood pooling.
- Heart Failure: Insufficient heart function can disrupt normal blood flow.
- Diabetes: Can cause vascular complications affecting circulation.
6. Trauma or Injury
Trauma to the legs or veins can impede blood flow and lead to stasis. Injuries can cause swelling and restrict normal circulation, especially if they involve fracture or significant soft tissue damage.
Recognizing the Symptoms of Venous Stasis
Identifying the symptoms of venous stasis is critical for prompt intervention. Common signs include:
- Swelling: Particularly in the legs and ankles, especially after prolonged standing or sitting.
- Pain or Aching: Discomfort in the affected areas, often worsening throughout the day.
- Skin Changes: Discoloration or changes in skin texture, such as dry or flaky skin.
- Ulcers: In severe cases, skin ulcers can develop due to poor circulation.
Impact of Venous Stasis on Health
If left untreated, venous stasis can lead to serious health complications, including:
- Deep Vein Thrombosis (DVT): A potentially life-threatening condition where blood clots form in deep veins.
- Chronic Venous Insufficiency: A long-term condition where veins cannot pump enough blood back to the heart.
- Skin Infections and Ulcers: Due to impaired blood circulation.
Preventive Measures and Treatment Options
Implementing preventive measures can significantly lower the risk of venous stasis. Here are some effective strategies:
1. Regular Physical Activity
Engaging in regular exercise promotes circulation and helps maintain a healthy weight. Consider activities that promote leg movement, such as:
- Walking or Jogging
- Swimming
- Cycling
2. Maintain a Healthy Weight
Achieving and maintaining a healthy weight can alleviate undue pressure on the veins. A balanced diet rich in fruits, vegetables, lean protein, and whole grains can support weight management.
3. Elevate Your Legs
Whenever possible, elevate your legs to promote better venous return. This can be particularly helpful after prolonged periods of sitting or standing.
4. Compression Stockings
Compression therapy helps support venous circulation by applying controlled pressure to the legs. This can significantly reduce the risk of stasis, particularly for individuals with a higher risk.
5. Hydration
Drinking adequate water helps maintain blood viscosity and supports overall circulatory health. It’s important to stay hydrated, especially during hot weather or strenuous exercise.
6. Medical Interventions
In some cases, medical treatment may be necessary. Options include:
- Medications: Anticoagulants may be prescribed to reduce the risk of clot formation.
- Surgical Procedures: For severe cases, surgical options may be considered, including vein stripping or valve repair.
Conclusion: Taking Action Against Venous Stasis
Understanding venous stasis causes and taking proactive measures can significantly enhance vascular health. By recognizing the risk factors, adopting preventive strategies, and seeking timely medical intervention if necessary, individuals can improve their quality of life and reduce the risk of severe complications. Whether you’re concerned about your health or someone else’s, awareness is the first step toward proactive vascular health management.
For personalized assessment and treatment options related to venous stasis, consider consulting a specialist. By prioritizing vascular health, you’re investing in your overall well-being.
For more information, visit trufflesveinspecialists.com.



